Fear says what if, Faith says even if.

The few minutes prior to taking my Midwive’s Brew, I stood in my bathroom with the shower water running, just breathing . It was June 20th, about 10:29am. I then said a prayer. It wasn’t a “please give me a perfect home birth” prayer. It was more of a “God, I trust you. Come what may” prayer. I don’t often ask for something too specific when I pray. More so, I ask for protection from what ever does come. I asked for whatever was meant to happen, to happen with His arms wrapped around me and my family for comfort and safety. I asked that if something were to happen to the baby, that we get through it. That if something happened to me, that Ben and Emery get through it. I asked for everyone to come out okay at the end of the day, one way or the other, with whatever were to happen.
And then I drank the Brew — castor oil, almond butter & mango juice — and took a shower. I was 41 and 4 days pregnant. I had completed a biophysical profile and a fetal non-stress test that week at the direction of my midwife and everything indicated that I was growing a healthy baby who just wasn’t coming out of the womb quite on his own quite yet. After two losses prior to this pregnancy, I was not comfortable going past 42 weeks. Prior to taking the Brew, I’d spent 7-10 days researching castor oil induction and I felt confident in my decision. I’d had a membrane sweep 2 days prior and at that time I was 3cm dilated. (The Brew should NOT be consumed if you’re not dilated. And should not be consumed before your due date. I had no bad reaction to the Brew. No nausea, no vomiting, no diarrhea.)
At approximately 12:35pm, after contractions had ramped up a bit but were not painful (I’d been having off and on strong contractions for a few days, with increased braxton hicks/occasional prodromal for 2 weeks straight), I was standing in the bathroom when my water broke. And then, my contractions went from not painful, to about 7/10 painful. I called my midwife and told her my water broke. She was on the phone with me during a contraction and I told her to give me a few more minutes and then I’d call her if I wanted her to come. I think I lasted 3 more contractions before Ben told her to come over and my contractions were more painful than they ever were with Emery. And I labored for 20 hours unmedicated with Emery while being stuck in transition for 6 hours. And these contractions were so much more powerful than any I had with her. My midwife had already packed all her things and was about to leave when Ben called. She only lives 10 minutes away. By the time she arrived literally only 10 mins later, my contractions were 2.5-3 minutes apart and I was on the floor hovering over the toilet to get through them.
The next hour went by in a blur. Here is what I remember:
My baby was coming. And fast. Contractions were so strong it was hard to breathe through them at all. I tried to relax in the birth pool but I was already feeling this overwhelming urge to push. I also felt like I needed to pee! And I couldn’t pee. In the bathroom my midwife attempted to straight cath me because I was so uncomfortable from being unable to pee and I asked her for help — even though it had only been maybe 3 hours since I last voided. And then something happened. My body felt the urge to push but the pain was overwhelming. As if something was wrong. My midwife listened to the HR of our little guy multiple times and all sounded well. Strong heart. But something in me changed. From the time my contractions started, something in me was thinking it didn’t feel right. Why was the pain so bad? Why was my baby still so high up in my belly? I could feel him. I could see him. He was HIGH. He was in a good position (LOA). Why wasn’t he coming down? I’m not sure how long I labored at home before I looked at my midwife and told her we needed to get to the hospital. Something wasn’t right. It was not a long time. I had this insane maternal instinct that I cannot explain. It was not fear. It was determination. And I didn’t quite know where it was coming from because I was at home, safe, where I wanted to birth and I was giving that up to do the one thing I didn’t want to do — go to a hospital.
Ben drove us to the hospital which is about 11 minutes away. Talk about misery. I refused to take a wheel chair up to OB because I was in too much pain to sit. I had contractions and my water leaked as I walked bare foot into the hospital, up the elevator, and down the halls to OB. When I arrived, one of the doctor’s I’d met previously was there waiting (my midwife had texted her) and the nurses immediately began annoying me with their questions. I ended up really liking them, but I think they underestimated the fact that 1. I know my body and 2. The baby was trying to come. No time for small talk.
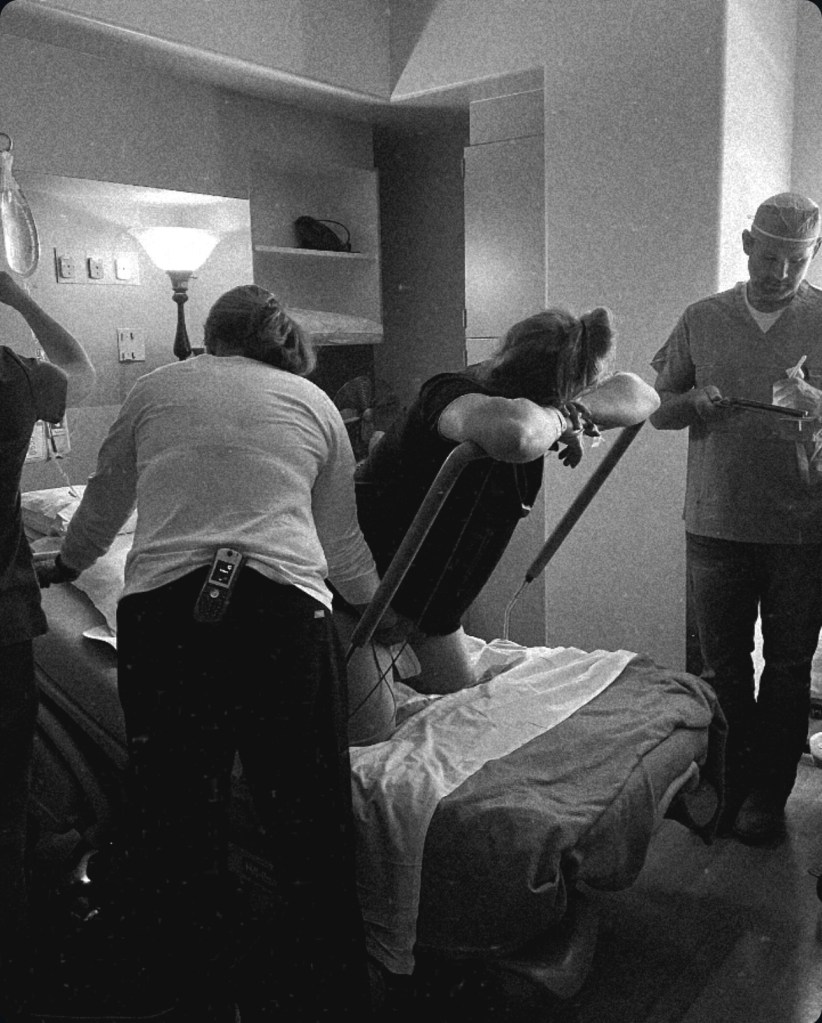
Pushing began mere minutes after I arrived. I held onto Ben with each contraction and push. As usual, he did not leave my side and I leaned on him for every single thing.
The pushing didn’t feel normal. Nothing felt normal. I get it, it’s labor. It is painful. But something was wrong. I can’t tell you how strong my mama instinct was that day. My midwife and I have discussed this extensively since, and she just thanks me each time. Thankful because she’s had women who ignored their instincts because they wanted a home birth so bad — and things got bad. Earlier that morning, she had told me she had never had such a strong feeling that it was time for a baby to come out. Why were we both feeling this way?
I had read a lot of birth prep literature, listened to podcasts, watched birth videos and filled my mind with positive thoughts of how capable my body was prior to June 20th. There is so much out there regarding interventions, medically managed pregnancies, unnecessary c-sections, etc. etc. and how you “just need to trust your body” and there I was, trusting my body despite wanting the opposite of what it was telling me.
Of course I wanted a home birth. I have been a nurse for 11 years. In hospitals. I hate hospitals. Did I have to give birth in one– again? But this time there was a difference. This time, I chose to seek medical care. With Emery, they made me leave the birth center. I was at 8cm, my body needed more time, and they made me. Convinced me to get an epidural. I will never get over that entire scenario. It took me a long time to fully process it. Yet this was different. My body was telling me to get to the hospital. For whatever reason, I sought medical care.
I continued pushing. And pushing. I asked for pain relief. But I was already 8+ cm. I kept asking. And then I was 9cm. Baby was +2 station. My body couldn’t stop pushing. It wasn’t me being told to push. My body was doing it all on its own. Every time a contraction would come on, I had to push. Of course, nothing was happening. Luckily they were able to straight cath me because I kept begging to pee – but only 200ml of tea colored urine came out. What?
At 9+ cm the MD agreed to allow the CRNA to give me the epidural. It was pretty interesting getting an epidural while pushing but not allowing your body to move. Thanks to the seasoned nurse for helping me through that scenario! Of course it took forever to even work. And forever I mean probably 20 minutes because all of this happened so fast. Time seemed like it was standing still — but things were moving so quickly. The epidural spreads best if you’re on your back, but babies heart rate started to decline while I was on my back (naturally– this can occur at home too when women sleep on their backs while pregnant), so I got on my knees and pushed that way, leaning over a bar. His heart rate recovered no problem. And it stayed great for a while. Until pushing became more frequent and I was pushing for longer time periods. After a while things took a turn. As a nurse who has been listening to hearts beating for years, I knew what some in the room were not saying. I knew his heart rate wasn’t recovering after the contractions. A dip in heart rate during a contraction is normal. The heart rate returning to a baseline beat per minute after the contraction is over is also normal. His wasn’t returning. At one point, he was hovering in the 50’s. And then the 60’s. And then he’d jump back up for a second and I thought, oh good! He’s back to 120’s! And then he’d dip. The tone in the room began to change. We needed to get the baby out. I pushed so hard. So, so hard. Each contraction I pushed. And I took a breath and I pushed again. And again. Nothing was happening. He was not coming lower down into the canal. We’d see hair — and then he’d slide right back up. I could feel his little body moving frantically in my upper belly. And I could hear that low heart rate for so long after the contraction stopped, just for another contraction to begin without his little heart recovering.
The doctor asked if she could try the vacuum. When I say I shot her a death look and said no immediately, I mean I shot her a death look and said no immediately. She asked my fears. We talked it through. I asked my midwife for guidance. My midwife agreed that the baby needed to come. We allowed the vacuum twice with zero progression before I made her stop and begged for a C-section. I looked her in the eyes and I said, “I need this baby to come out. Please take me to the OR.” And she did.
In that moment NOTHING was more important to me than delivering my boy before his heart dipped lower.
In the OR I was awake and talking to the Nurse Anesthetist the entire time. I screamed when they began cutting me open. I could feel sharp pain in my lower left side. He gave me Fentanyl only after asking if he could give me the Fentanyl. The upside of being a nurse is you have the respect and attention of the staff serving you maybe a bit more than if I didn’t know my meds and vitals and abnormalities.

It seemed as if just as soon as I was screaming over the pain of the cut that I heard everyone yell that he was out and okay. It was like 2 minutes. How can a baby come out so fast??? Ben was there discussing everything with me but of course having been lying flat and unable to see much, I couldn’t exactly understand all that was going on. Mostly I felt the tug and tug and tug of the c-section. How weird is it to have your abdomen sliced open, baby removed, your body irrigated and then all put back together again in a few minutes time? While you’re awake?
All I cared about was if he was okay. He was better than okay. APGAR’s of 8 and 9. There was a little moment where he stopped breathing there (this is not abnormal — babies can get “stunned” after they enter our big wild world and this can happen after they come out crying). At home, I would have birthed him and brought him to my chest. I would have rubbed him if he needed it, or given him a small breath to get him to breathe on his own. In the hospital they put a mask on his face. Even if only for a moment, they did. And then his oxygen sats were 97% and he was taking breaths and he was okay.
Such is life you guys. I am a medical provider. I know how this works. You help the patient with your standard medical resources. I forfeited the opportunity to be the one to help my baby into the world the moment I sought medical care and asked for the c-section. For the situation we were in, I do not regret it for a second.
Ben brought our baby boy to me. Tears. I just remember tears.
And then I hemorrhaged. My BP dropped to 80’s over 40’s. They gave me some other medication – I can’t remember what it was – and then I argued with them over the amount of Pitocin I was going to receive. You know me, always wanting minimal interventions even in the event of a ton of interventions 😉 (I won out, by the way. The Pit was stopped shortly after I returned to my room). My blood pressure recovered in about an hour after the blood loss and my color came back. I was ok.

In the recovery room the nurse helped me get the baby to latch. Which he did, right away. After having a baby previously who was never able to effectively latch, you cannot imagine my relief that he latched right away after all of that. More tears.
Once back to my room, Emery was waiting for her mama with our midwife’s assistant who had taken on the roll of Emery’s nanny during this entire time. Thank you GOD. Truly. Thank you God for her devotion to me and my family during this time. She watched Emery at our house and drove her to the hospital. It just so happens that she has a daughter Emery’s age, and a car seat for her size. She was there to assist a midwife and she took on a far different role. That is the kind of personalized care that I sought when wanting a home birth. Watching my first baby meet our new baby was overwhelming. I will never forget that moment. It made the past several hours pale in comparison to that overwhelming emotion of love for my children.

I look back on this day with peace. Of course there are things I am not too happy about overall (like, ummmm, having a C-section?). But I am so much more at peace about this birth than Emery’s. I chose to seek medical care. I chose to ask for a C-section (this is true, even if I already know it was on the horizon. It just felt better being the one to ask for it.). I made my own informed decisions. Now in hindsight I kind of wish I would have been more prepared for an emergency c-section because there are things I would have done differently ie. asked for immediate skin to skin. But the c-section was emergent in a tiny 25 bed hospital in rural Colorado with limited staff. I was their priority that day. And I was treated like it. Everything happened so, so fast. And simultaneously it was so low key. How is that possible? I don’t know. Small town stuff, I suppose.
I sit here today, 10 days post-op…. and I can’t believe the day of June 20th. Less than 5.5 hours after my water breaking I was in the recovery room holding my perfect son. My body took a beating with all of the pushing and then surgery. But today we are making our way through this postpartum period together. It didn’t start out how I planned. Postpartum hasn’t gone as planned. But he is so healthy so far, and I am able to breastfeed him with a healthy supply. He’s a big boy — born at 9lbs and 14.4 oz and he’s a hungry boy — and our breastfeeding journey has been beautiful.
The doctor came to visit the day after the birth. I thanked her. She was not pushy. She explained everything. She offered suggestions and options during the birth and she listened to me. My doula had said that she really wished all doctors were like her. How blessed I am that she was mine.
She did tell me a couple of interesting things that next day. 1. His cord was not an issue. It wasn’t wrapped around anything. It was just…. there. 2. His head was perfectly shaped. In many cases with an emergent c-section that comes after hour(s) of pushing, the babies head comes out completely misshapen. Not this babies. Why? Because his head wasn’t even descending. We will never know what was going on in my pelvis that day. But I know in my heart and my gut that I made the right decision to surrender and have the c-section.
Now, with all of this being said, it’s time for some real talk. Recovery has been a B* and I have absolutely no idea how or why so many women CHOOSE to have a c-section. I would never want to go through this again. Ever. Give me a vaginal birth and recovery PLEASE any day over what I’ve gone through in these past 10 days.
But…. he’s here. And he’s healthy. And I’m here. And I’m healthy. And at the end of the day…. I can say that while I got the c-section I never wanted instead of my home birth, I truly feel at peace about it all. I guess that’s what trusting your body and your mind really is all about. A lot of people say, Oh well the baby is here and that’s all that matters! I’m not going to say that. Of course ultimately you just want your healthy baby in your arms. But for those of us who spent months and years studying and preparing, we want a bit more. I’m not just referring to a home birth. I’m referring to the peace relating to the birth story.
My midwife said to me — “Wow, you had a home birth, hospital and emergent situation with surgery experience all in one birth story.” And I guess I did.
Humbling.

What a story!!!! You were the most prepared woman I’ve ever known but as we know…..we plan, God laughs! So happy it all turned out well and you have your little Archie to snuggle up to his big sister! Love you all.